| Saleptsis Vasileios Vascular Surgeon - Ph.D., University of Thessaly |
Our Services:
Doctor Saleptsis has a rich and constantly evolving, professional experience and he's able to offer you solutions for medical matters that has to do with:
| Coloured vascular ultrasound - triplex |
|---|
|
Certified practician of vascular ultrasound by the Central Health Council (KSY) |
| Lower Limb Varicose Veins - Spider - Veins Telangiectasias |
|
Usual signs to make a therapeutic intervention of varicose veins are:
The aim of surgery is to reduce blood pressure in the veins beneath the skin. Removing damaged veins helps the smooth and unhindered return of blood to the heart.The surgery is effective in controlling symptoms, preventing complications of varicose veins and emerging of new varicose veins.
Varicose veins will not subside on their own or using ointments, medicines, etc., but only through therapeutic intervention. If small varicose veins cause no symptoms though, there's no need to be cured but can be treated perfectly only for aesthetic reasons. Since the late '90s, new surgical methods for the treatment of varicose veins of the lower limb has emerged, which are considered less invasive, but also requires surgical incisions to remove the infected veins. The difference is that there's extirpation of the saphenous vein, but with administration of thermal energy directly to the inner wall through a flexible catheter (which is placed into the vein) and heat catalyzing is applied (thermal ablation). That results the development of fibrosis, i.e. replacement of the vein from gingival connective tissue, and finally the absorption of the vein by the body. These techniques are possible without general anesthesia, but require local (tumescent) anesthesia. Ιn cases of thermal ablation, vein removal also required with microtomes and is applied compression bandage to the member from the toes to the groin. Of course some limitations has to be explained in detail in patients before thermal ablation chosen as a treatment method. |
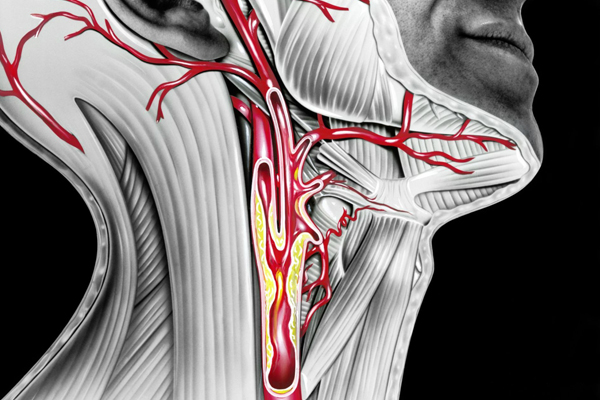
| Carotid Disease |
|
Carotid disease is the narrowing or occlusion of the carotid arteries, usually due to atherosclerosis (hardening of the arteries). The carotid arteries are two large blood vessels, one on each side of the neck, which supplies blood (oxygen and nutrients) to the front part of the brain. Carotids perfuses the part of the brain that controls thought, speech, personality, sensory and body mobility. The progression of carotid disease can result in a significant narrowing of the lumen, or atherosclerotic plaque rupture and coagulant release which can lead to blood flow in smaller arteries of the brain, and to occlude. As a result of the reduction or stop of blood flow, in other words, the interruption of oxygen supply to the brain, leads to "choking" and eventually destruction of brain cells. This is called ischemic stroke, when the brain damage is permanent, or TIA when the disturbance of cerebral function is temporary. The carotid disease is associated with approximately one third of strokes. There are also some other stroke causes such as atrial fibrillation (arrhythmia of the heart), atherosclerosis of the small vessels of the brain or intracranial haemorrhage.
Ways of dealing with the disease:
|
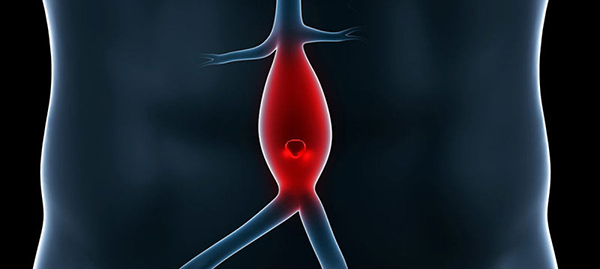
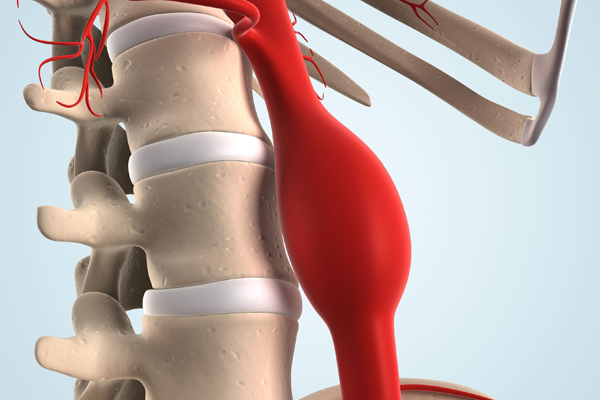
| Aneurysmal Disease |
|
Aneurysm is the condition where the diameter of the vessel part is at least 1.5 times greater than the continuous healthy part of the same vessel, or the diameter of the largest healthy patient's vessel. The most common cause of inducing this disease, is atherosclerosis (> 50%).
The endovascular repair of abdominal and thoracic aortic anerysmaton has become a routine procedure in recent years. For implementing this method, there are some specific anatomical conditions such as restriction of the aneurysm of the abdominal aort at the level below the outgrowth of the renal arteries and restriction of the aneurysm of the thoracic aorta at the level above the origin of the celiac artery and mesentery. The only treatment of aneurysms which reach neurite renal artery (flare), higher (over kidney or hyperkidney) and the thoracoabdominal, is the open surgical procedure, which is accompanied by significant morbidity (such as renal failure and paraplegia) and mortality even in specialized centers abroad. To succesfully address these types of aneurysms, a relatively new in our country method, but applied for years in a few centers in the world (fenestrated - branched technique), based on integration into the main endovascular graft upon request, holes (ports) and lateral small cuttings (branches) corresponding to the points of neurite visceral arteries of the abdominal aorta (renal, mesenteric and upper abdominal artery). Through holes and those gavaged viscera vessels branches, which are ensured and reperfused with new smaller intravascularly grafts (Stents and angioplasty). |
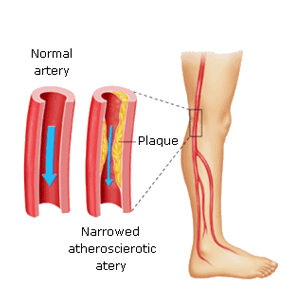
| Peripheral Arterial Disease |
|
Normally arteries are smooth in the interior, but with aging the inside wall may become thick and uneven due to deposition of materials such as cholesterol, calcium, damaged cells and fibrous tissue. These deposits are called plaque, which is something similar to "tartar" of water pipes. This is atherosclerosis. A plate may be complicated by bleeding internally, by cutting and pasting of blood clots. The complicated atherosclerosis can narrow an artery (stenosis) or close it completely (obstruction). Atherosclerosis tends to appear in places where arteries branch off. The arteries carry oxygenated blood and nutrients from the heart to the rest of the body. hen accumulated enough plate, to a degree sufficient to reduce the blood flow and oxygen to the bottom members, i.e. when occur stenosis or occlusion of arteries that supply blood, this condition is called peripheral arterial occlusive disease (PID), or peripheral vascular disease (PAN). The arteries that may be affected in the PID is the abdominal aorta, the iliac, femoral, popliteal and the tibial arteries.
Some ways of dealing with the disease:
|
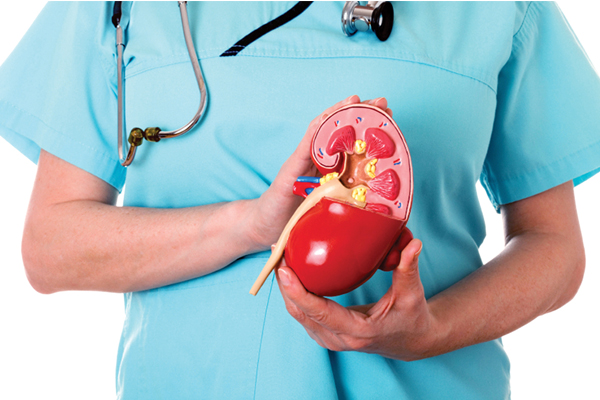
| Chronic Renal Failure |
|
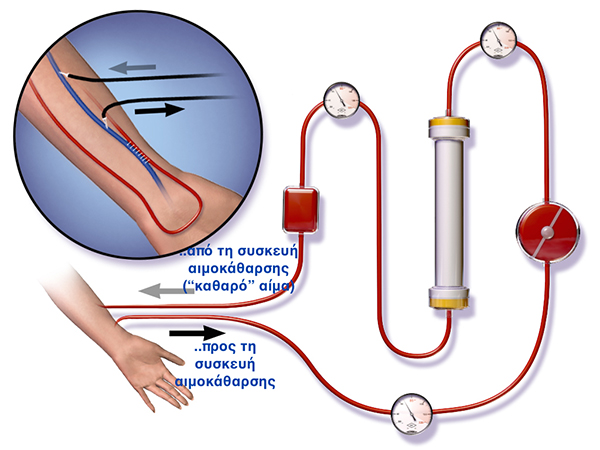
Chronic renal failure is progressive, irreversible decrease on renal function, which is caused by damage of various genesis kidney. Chronic renal failure starts gently and can reach up to end-stage renal failure, a process that can last from 2 to 10 years. In the final stage of the disease the patient needs immediate support of renal function by hemodialysis or peritoneal dialysis.
Arteriovenous Communication - Fistula The fistula is usually created in the nondominant hand, usually in the forearm (radial artery to the cephalic vein) or above the elbow (brachial artery to cephalic vein). A fistula needs a long time to cure (approximately two to three months). During the dialysis, two needles entering the fistula, one to draw blood and one to return it. Advantages of Arterio-venous communication is the low incidence of infections, because it contains no foreign matter, it permits -due to it's construction- of high flows (which translates into more active hemodialysis) and a low incidence of thrombosis. There are few complications, but if the fistula is high flow and the vasculature that supports the arm rest is poor, can occur a so-called pilfer syndrome wherein blood entering the end is pulled towards the fistula and returns to the general circulation without perfusion hand rest. This causes a cold hand, painful cramping and in some occasions, tissue ischemia. A Long Term complication is an aneurysm progression, a stretching of the vein wall which is weakened by the repeated insertion of needles. In order to reduce the risk of aneurysm it must applied the rotation of the puncture. Aneurysms may require surgical correction and can shorten the operating life time of fistula.
Hemodialysis graft They mature faster than the fistula and may be ready in a few weeks after the formation or even sooner. But they have a high risk for stenosis that can lead to a clot and thrombosis. As a foreign material can be contaminated easily. Finally they can be placed in more locations because they have great length as the thigh or in the cervix. |
| Diabetic Foot |
|
Recently, in order to treat patients and reduce amputations, the medical community has turned with great interest to the disease called "diabetic foot".
A single wound can lead to amputation of diabetic foot!
At international level, every 30" the leg of a diabetic is being amputated. In Greece, amputation of one or both legs, are about 2.500-3.500 of the cases! The diabetic foot belongs to a man who suffers from chronic diabetes. The usual occurrence of a diabetic foot occurs after at least 10 to 15 years unregulated diabetes and it's more common in diabetic type 1, to those required insulin for their treatment since the pancreas is not operating. Prevention and proper counseling by the physician is extremely important for a diabetic patient. Many diabetics are not sufficiently informed about their disease or the possible consequences of diabetes on their feet. More than 70% of patients experienced problems with their feet. Mr. Saleptsis and his specialised team, can fully treat a diabetic foot. The team consist of a Vascular Surgeon, Orthopedic, Endocrinologist and Dermatologist. |
      |